Needs analysis for maxillofacial surgery‑specific operating rooms at the University of Port Harcourt Teaching Hospital, Nigeria
Main Article Content
Abstract
Background: Acquiring experience and surgical skills in maxillofacial surgery and anaesthesia depend on an optimal case volume and case mix. The more opportunities available for hands-on participation in various surgical operations, the better for the maxillofacial surgical team. Building and equipping operating rooms (ORs) are high-cost intensive projects. The aim of this study was to find if the current operative case mix and volume justifies capital investment in maxillofacial surgery-specific ORs.
Methods: This is a descriptive, nonexperimental quantitative research. We reviewed the maxillofacial OR records from November 2008 to December 2013. Data collected from the maxillofacial theatre records were incorporated into an SPSS v 22 spreadsheet and analysed. The OR utilisation time was computed. The analysis was performed to guide managerial and investment decisions.
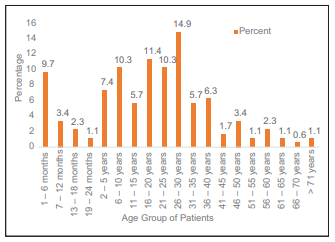
Results: A total of 175 maxillofacial operative cases reviewed from a period of 62 months gave a rate of 2.8 cases per month. More males 90 (51.4%) than females 85 (48.6%) were operated on. Of the 236 operating days, 129 days(54.7%) were utilised. Major and major/smile-train operations formed 73.7% of all operations performed. All operations started after 10 am.
Conclusion: The maxillofacial case volume and output do not justify the need for capital investment into building surgery-specific ORs. However, there is a need to improve OR management and put in place strategies that will optimise the present facility.
Downloads
Article Details
The journal grants the right to make small numbers of printed copies for their personal non-commercial use under Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported License.
References
1. Onajin‑Obembe B. From service to academics: Analysis of a change process in the department of anaesthesiology, University of Port Harcourt Teaching Hospital (UPTH), Nigeria. Int J Manag Bus Stud 2013;3:110‑7.
2. Macario A, Vitez TS, Dunn B, McDonald T. Where are the costs in perioperative care? Analysis of hospital costs and charges for inpatient
surgical care. Anesthesiology 1995;83:1138‑44.
3. Jackson RL. The business of surgery. Managing the OR as a profit center requires more than just IT. It requires a profit‑making mindset, too. Health Manag Technol 2002;23:20‑2.
4. Oh HC, Phua TB, Chuen S, Yen Lim JF. Assessing the performance of operating rooms: What to measure and why? Proc Singapore Healthc
2011;20:105‑9.
5. Marjamaa R, Vakkuri A, Kirvelä O. Operating room management: Why, how and by whom? Acta Anaesthesiol Scand 2008;52:596‑600.
6. Weinbroum AA, Ekstein P, Ezri T. Efficiency of the operating room suite. Am J Surg 2003;185:244‑50.
7. Gallagher AG, Ritter EM, Champion H, Higgins G, Fried MP, Moses G, et al. Virtual reality simulation for the operating room: Proficiency‑based training as a paradigm shift in surgical skills training. Ann Surg 2005;241:364‑72.
8. Roberts KE, Bell RL, Duffy AJ. Evolution of surgical skills training. World J Gastroenterol 2006;12:3219‑24.
9. Ciechanowicz S, Wilson N. Delays to operating theatre lists: Observations from a UK centre. Internet J Health 2010;13:1. Available from: https://www.ispub.com/IJH/13/1/6740. [Last accessed on 2018 Jun 03].
10. Wong J, Khu KJ, Kaderali Z, Bernstein M. Delays in the operating room: Signs of an imperfect system. Can J Surg 2010;53:189‑95.
11. Thorburn H, Khanna S, Boyle J, Good N, Steyn M. Analysis of operating theatre utilisation to drive efficiency and productivity improvements. Stud Health Technol Inform 2014;204:163‑8.