Effect of cigarette smoking on salivary electrolyte composition in a sub‑urban Nigerian population
Main Article Content
Abstract
Background: Cigarette smoking is a factor that affects the health of humans. It has been shown to be an important risk factor for a variety of disorders such as disease of the lungs, brain damage and has also been linked to the development of periodontal disease. There are, however, few and conflicting studies on its effect on salivary electrolyte composition.
Aim: The aim of this study is to evaluate the effect of chronic cigarette smoking on electrolyte concentration of saliva and to determine its effect on normal oral homeostasis.
Methods: A total of 40 male subjects of between 25–40 years were divided into two groups, A and B. Group A comprised of 20 smokers and Group B, 20 non-smokers. Saliva from each subject was collected into a plain sample bottles and immediately analysed.
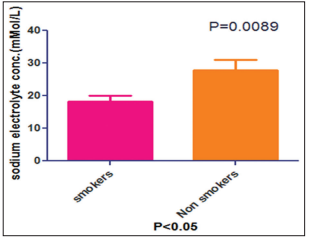
Results: Results showed a significantly lower concentration of Na+ and Cl− and a significantly higher HCO3 − and K+ in smokers than non-smokers.
Conclusion: This shows that the concentration of electrolytes in the saliva may be affected by the chronic use of tobacco which could have adverse consequences on the normal homeostasis of the oral environment especially with regard to increased salivary alkalinity as a result of increased salivary bicarbonate.
Downloads
Article Details
The journal grants the right to make small numbers of printed copies for their personal non-commercial use under Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported License.
References
1. Doll R, Peto R, Wheatley K, Gray R, Sutherland I. Mortality in relation to smoking: 40 years’ observations on male British doctors. BMJ 1994; 309: 901‑11.
2. Proctor RN. Tobacco and the global lung cancer epidemic. Nat Rev Cancer 2001;1:82‑6.
3. Singh CR, Kathiresan K. Effect of cigarette smoking on human health and promising remedy by mangroves. Asian Pac J Trop Biomed 2015; 5: 162‑7.
4. Carpenter GH. The secretion, components, and properties of saliva. Annu Rev Food Sci Technol 2013;4:267‑76.
5. Edgar WM. Saliva: Its secretion, composition and functions. Br Dent J 1992;172:305‑12.
6. Liu J, Duan Y. Saliva: A potential media for disease diagnostics and monitoring. Oral Oncol 2012;48:569‑77.
7. Nunes LA, Mussavira S, Bindhu OS. Clinical and diagnostic utility of saliva as a non‑invasive diagnostic fluid: A systematic review. Biochem
Med (Zagreb) 2015;25:177‑92.
8. Kidwell DA, Holland JC, Athanaselis S. Testing for drugs of abuse in saliva and sweat. J Chromatogr B Biomed Sci Appl 1998;713:111‑35.
9. Javaid MA, Ahmed AS, Durand R, Tran SD. Saliva as a diagnostic tool for oral and systemic diseases. J Oral Biol Craniofac Res 2016;6:66‑75.
10. de Almeida Pdel V, Gr, Gr AM, Machado MA, de Lima AA, Azevedo LR. Saliva composition and functions: A comprehensive review. J Contemp Dent Pract 2008;9:72‑80.
11. Kallapur B, Ramalingam K, Bastian, Mujib A, Sarkar A, Sethuraman S. Quantitative estimation of sodium, potassium and total protein in
saliva of diabetic smokers and nonsmokers: A novel study. J Nat Sci Biol Med 2013;4:341‑5.
12. Maier H, Born IA, Mall G. Effect of chronic ethanol and nicotine consumption on the function and morphology of the salivary glands. Klin Wochenschr 1988;66 Suppl 11:140‑50.
13. Eliasson M, HM, E, Lundblad D, Karlsson R, Bucht E. Influence of smoking and snuff use on electrolytes, adrenal and calcium regulating
hormones. Acta Endocrinol (Copenh) 1993;128:35‑40.
14. Laine MA, Sewne LA, Karjalainen SM, Helenius H, Doroguinskaia A, Lehtonen‑Veromaa M, et al. Salivary variables in relation to tobacco
smoking and female sex steroid hormone‑use in 30 to 59‑year‑old women. Acta Odontol Scand 2002;60:237‑40.
15. Erdemir EO, Erdemir A. The detection of salivary minerals in smokers and non‑smokers with chronic periodontitis by the inductively coupled
plasma‑atomic emission spectrophotometry technique. J Periodontol 2006;77:990‑5.
16. Avşar A, Darka O, Bodrumlu EH, Bek Y. Evaluation of the relationship between passive smoking and salivary electrolytes, protein, secretory
IgA, sialic acid and amylase in young children. Arch Oral Biol 2009;54:457‑63.
17. Axelsson P, Paulander J, Lindhe J. Relationship between smoking and dental status in 35‑, 50‑, 65‑, and 75‑year‑old individuals. J Clin Periodontol 1998;25:297‑305.
18. Singh M, Ingle NA, Kaur N, Yadav P, Ingle E. Effect of long‑term smoking on salivary flow rate and salivary pH. J Indian Assoc Public Health Dent 2015;13:11.
19. Padmavathi P, Reddy VD, Varadacharyulu N. Influence of chronic cigarette smoking on serum biochemical profile in male human volunteers. J Health Sci 2009;55:265‑70.
20. Jessie K, Pang WW, Haji Z, Rahim A, Hashim OH. Proteomic analysis of whole human saliva detects enhanced expression of interleukin‑1 receptor antagonist, thioredoxin and lipocalin‑1 in cigarette smokers compared to non‑smokers. Int J Mol Sci 2010;11:4488‑505.
21. Tenovuo J, , Lagerlöf F. Saliva. In: Thylstrup A, Fejerskov O, editors. Textbook of Clinical Cardiology. 2nd ed., Ch. 2. Copenhagen, Denmark:
Munksgaard, 1994; 17‑43.
22. Khan GJ, Javed M, Ishaq M. Effect of smoking on salivary flow rate. Gomal J Med Sci 2010;8:221‑4.
23. Ertu2180 F, Elbek‑Cubukub C, Sabah E, Mir S. The oral health status of children undergoing hemodialysis treatment. Turk J Pediatr 2003; 45: 108‑13.
24. Baliga S, Muglikar S, Kale R. Salivary pH: A diagnostic biomarker. J Indian Soc Periodontol 2013;17:461‑5.
25. Tomar SL, Asma S. Smoking‑attributable periodontitis in the United States: Findings from NHANES III. J Periodontol 2000;71:743‑51.