Prevalence and pattern of inflammatory dermatoses and skin cancers in highly active antiretroviral therapy‑experienced and highly active antiretroviral therapy‑naive patients in the University of Benin Teaching Hospital, Benin City, Nigeria
Main Article Content
Abstract
Introduction: Highly active antiretroviral therapy (HAART) reduces morbidity, mortality and prolong life in patients with human immunodeficiency virus (HIV) infection. Only a few studies have compared the prevalence and pattern of inflammatory dermatoses and skin cancers in HAART-naïve and HAART-experienced HIV-infected patients.
Aim: The aim of this study was to determine the prevalence and pattern of inflammatory dermatoses and skin cancers in HAART-experienced and HAART-naive patients in the University of Benin Teaching Hospital, Benin City, Nigeria.
Methods: This was a comparative cross-sectional study that involved 330 HAART-experienced patients and 330 HAART-naive patients. Patients were examined for inflammatory dermatoses and skin cancers. Skin biopsies were done where applicable for diagnostic accuracy.
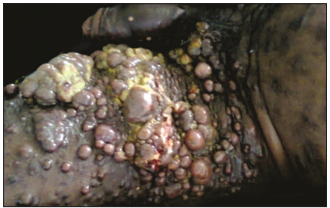
Results: The mean age of the HAART-experienced group and HAART-naïve group was 42.39 ± 10.1 years and 39.9 ± 11.2 years, respectively. The male-to-female ratio of the HAART-naive and HAART-experienced population was 1.9:1 and 3:1, respectively. The median CD4 count of the HAART-naive group was significantly lower than the HAART-experienced group (275.5 vs. 487 cells/µ P ≤ 0.01). Skin cancers were present in 1.8% of the HAART-naïve group but absent in HAART-experienced patients (P ≤ 0.01). The prevalence of inflammatory dermatoses was 36 (10.9%) in the HAART-naïve group and 8 (2.4%) in the HAART-experienced group (P < 0.01). Pruritic papular eruption was the most common inflammatory dermatoses in both groups with a prevalence of 7.6% and 1.2% in the HAART-naïve and HAART-experienced groups, respectively.
Conclusion: Inflammatory dermatoses and skin malignancies were more common in HAART-naive HIV-infected patients compared to HAART-experienced patients. HAART may reduce the cutaneous morbidity in HIV patients.
Downloads
Article Details
The journal grants the right to make small numbers of printed copies for their personal non-commercial use under Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported License.
References
1. Grayson W. The HIV‑positive skin biopsy. J Clin Pathol 2008;61:802‑17.
2. GargT, Sanke S. Inflammatory dermatoses in human immunodeficiency virus. Indian J AIDS 2017;38:113‑20.
3. Crum‑Cianflone N, Hullsiek KH, Satter E, Marconi V, Weintrob A, GanesanA, et al. Cutaneous malignancies among HIV‑infected persons.
Arch Intern Med 2009;169:1130‑8.
4. FearfieldLA, NelsonM, FrancisN, BunkerCB. Cutaneous squamous cell carcinoma with zosteriform metastases in a human immunodeficiency
virus‑infected patient. Br J Dermatol 2000;142:573‑4.
5. Ramadhan L, Mwenzi O, Onyango O, HyweiC, Aluoch J. Epidemiology and clinical spectrum of cutaneous diseases manifesting among newly
diagnosed HIV seropositive adults in Nakuru country Kenya. Cont J Med Res 2013;7:1‑9.
6. Umoru D, Oviawe O, Ibadin M, Onunu A, Esene H. Mucocutaneous manifestation of pediatric human immunodeficiency virus/acquired
immunodeficiency syndrome (HIV/AIDS) in relation to degree of immunosuppression: A study of a West African population. Int J Dermatol 2012; 51:305‑12.
7. Pitche P, Tchangaï‑Walla K, Napo‑Koura G, Mijiyawa M, Agbere A, Tatagan A, et al. Prevalence of skin manifestations in AIDS patients in the Lome‑Tokoin university hospital (Togo). Sante 1995;5:349‑52.
8. Puttaiah K, Sunith V. A hospital based cross sectional study of mucocutaneous manifestation in the infected. Int J Col Res Public Health 2010;3:1.
9. Bonita R, Beaglehole R. Basic Epidemiology. 2nd ed., Vol. 4. Geneva: World Health Organization; 2006. p. 81.
10. DermNet NZ’s. Dermoscopy of Other Non‑Melanocytic Lesions. Available from: http://www.dermnetnz.org/news.html. [Last accessed
on 2013 Oct 31].
11. Cheng ST, Ke CL, Lee CH, Wu CS, Chen GS, Hu SC, et al. Rainbow pattern in Kaposi’s sarcoma under polarized dermoscopy: A dermoscopic pathological study. Br J Dermatol 2009;160:801‑9.
12. Parkin JM, Eales LJ, Galazka AR, PinchingAJ. Atopic manifestations in the acquired immune deficiency syndrome: Response to recombinant
interferon gamma. Br Med J (Clin Res Ed) 1987;294:1185‑6.
13. Toback AC, Longley J, Cardullo AC, Doddy U, Romagnoli M, DeLeo VA, et al. Severe chronic photosensitivity in association with acquired immunodeficiency syndrome. J Am Acad Dermatol 1986;15:1056‑7.
14. Gillett J. The mosquito: Its life activities and impact on human affairs. In: Gillett J, editor. Mosquitoes. 1st ed. U.S, Garden city, NY: Double
Day; 1972. p. 313‑48.
15. Simons FE, Peng Z. Skeeter syndrome. J Allergy Clin Immunol 1999;104:705‑7.
16. Wichai S, Varuie D, Chasire S, Pornchai C, Nyunt N. Cutaneous morbidity in HIV positive patients. South East Asian J Trop Med Public Health 2001;32:1. Seborrheic Dermatitis. Available from: http://www. cumc.columbia.edu/dept/derm/conditions/sebo. [Last accessed on 2014 Jan 05].
17. Muhammad B, Eligius L, Mugusi F, Aris E, Chale S, Magao P, et al. The prevalence and pattern of skin diseases in relation to CD4 counts
among HIV‑infected police officers in Dares Salaam. Trop Doct 2003;33:44‑8.
18. NnorukaEN, Chukwuka JC, AnisuibaB. Correlation of mucocutaneous manifestations of HIV/AIDS infection with CD4 counts and disease
progression. Int J Dermatol 2007;46 Suppl 2:14‑8.
19. Sivayathorn A, Srihra B, Leesanguankul W. Prevalence of skin disease in patients infected with human immunodeficiency virus in Bangkok,
Thailand. Ann Acad Med Singapore 1995;24:528‑33.
20. Mbulaiteye SM, Bhatia K, Adebamowo C, Sasco AJ. HIV and cancer in Africa: Mutual collaboration between HIV and cancer programs may
provide timely research and public health data. Infect Agent Cancer 2011;6:16.
21. Onunu AN, Okoduwa C, Eze EU, Adeyekun AA, Kubeyinje EP, Schwartz RA, et al. Kaposi’s sarcoma in Nigeria. Int J Dermatol 2007;46:264‑7.
22. Salami T, Adewuyi G, Echekwube P, Affusim C. Pattern of cutaneous morbidity among a cohort of HIV/AIDS patients accessing care in Rural/Suburban adult ART clinic in Nigeria. Br J Dermatol 2013;3:1199‑207.
23. Josephine M, Issac E, George A, Ngole M, Albert SE. Patterns of skin manifestations and their relationships with CD4 counts among HIV/AIDS patients in Cameroon. Int J Dermatol 2006;45:280‑4.
24. Wamburu G, Masenga EJ, Moshi EZ, Schmid‑Grendelmeier P, Kempf W, Orfanos CE, et al. HIV‑associated and non‑ HIV associated types of Kaposi’s sarcoma in an African population in Tanzania. Status of immune suppression and HHV‑8 seroprevalence. Eur J Dermatol 2006;16:677‑82.
25. Knowles DM, Cesarman E. The Kaposi’s sarcoma‑associated herpesvirus (human herpesvirus‑8) in Kaposi’s sarcoma, malignant lymphoma, and other diseases. Ann Oncol 1997;8 Suppl 2:123‑9.
26. Mbulaiteye SM, Parkin DM, Rabkin CS. Epidemiology of AIDS‑related malignancies an international perspective. Hematol Oncol Clin North
Am 2003;17:673‑96, v.