Knowledge and perception of healthcare providers towards palliative care in Rivers State, Nigeria
Main Article Content
Abstract
Background: Palliative care, a multidisciplinary approach to specialised medical care, focuses on improving the quality of life for both the patient and the family. It increases their satisfaction and improves clinical outcome. Its concept, however, is relatively new in Nigeria, with services mainly limited to patients who attend the tertiary hospitals.
Aim: The aim of this study is to evaluate the knowledge and perception towards palliative care among health-care providers in Rivers State.
Methods: This cross-sectional study was conducted in November 2012 at the University of Port Harcourt Teaching Hospital, among participants of a workshop on Hospice and Palliative care. Participants were healthcare providers from within and outside the hospital, including doctors, nurses, pharmacists, social workers, medical and nursing students. A structured, anonymous and self-administered questionnaire was used to obtain data on knowledge of palliative care and awareness information. Data were analysed using SPSS version 20.0.
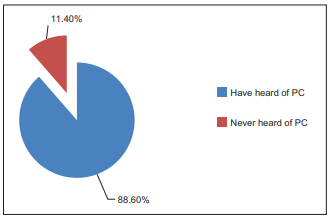
Results: There were 114 respondents and this comprised of 29 (25.4%) males and 85 (74.6%) females, giving a male-to-female ratio of 1:3. They were mainly doctors (44.7%) and nurses (44.7%). Majority (88%) had previously heard of palliative care. Sixty-four (56.1%) of them heard of it in a hospital setting from doctors/nurses, 37 (32.5%) from friends/family and 10 (8.8%) in school. Forty-six (40%) respondents believed that nurses should be the ones to provide palliative care services, while 32 (28%) believed the doctors should. Less than half (47.4%) were aware of the interdisciplinary facet of palliative care. Ninety-five (83.3%) respondents believed that terminally ill patients should benefit from palliative care services, while 17.5% believed that patients with diabetes should. More doctors (80%) than nurses (47%) rightly identified the components of palliative care.
Conclusion: Healthcare providers had insufficient knowledge concerning the interdisciplinary nature of the palliative care team, potentials beneficiaries and components of palliative care.
Downloads
Article Details
The journal grants the right to make small numbers of printed copies for their personal non-commercial use under Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported License.
References
1. Meiring MA. Caring for children with life‑limiting and life‑threatening illnesses: What the GP should know. Contin Med Educ 2011;29:286,
288-90.
2. Rodriguez KL, Barnato AE, Arnold RM. Perceptions and utilization of palliative care services in acute care hospitals. J Palliat Med 2007;10:99‑110.
3. Fraser LK, Miller M, Hain R, Norman P, Aldridge J, McKinney PA, et al. Rising national prevalence of life‑limiting conditions in children in England. Pediatrics 2012;129:e923‑9.
4. De Lima L. Palliative care and pain treatment in the global health agenda. Pain 2015;156(Suppl 1):S115‑8.
5. Morrison RS, Augustin R, Souvanna P, Meier DE. America’s care of serious illness: A state‑by‑state report card on access to palliative care in our nation’s hospitals. J Palliat Med 2011;14:1094‑6.
6. Fadare JO, Obimakinde AM, Afolayan JM, Popoola SO, Aduloju T, Adegun PT, et al. Healthcare workers knowledge and attitude toward
palliative care in an emerging tertiary centre in South-West Nigeria. Indian J Palliat Care 2014;20:1‑5.
7. Merriman A. Palliative care in Africa. Aortic News 2015;30:3‑6.
8. World Health Organization. WHO African Region Ministerial Consultation on Noncommunicable Diseases. Hosted in Brazzaville by the WHO/AFRO; April, 2011.
9. Fadare JO, Obimakinde AM, Olaogun DO, Afolayan JM, Olatunya O, Ogundipe KO. Perception of nurses about palliative care: Experience from South‑West Nigeria. Ann Med Health Sci Res 2014;4:723‑7.
10. Ahmed N, Bestall JC, Ahmedzai SH, Payne SA, Clark D, Noble B, et al. Systematic review of the problems and issues of accessing specialist palliative care by patients, carers and health and social care professionals. Palliat Med 2004;18:525‑42.
11. Kassa H, Murugan R, Zewdu F, Hailu M, Woldeyohannes D. Assessment of knowledge, attitude and practice and associated factors towards palliative care among nurses working in selected hospitals, Addis Ababa, Ethiopia. BMC Palliat Care 2014;13:6.
12. Abu‑Saad Huijer H, Dimassi H. Palliative care in Lebanon: Knowledge, attitudes and practices of physicians and nurses. J Med Liban 2007; 55: 121‑8.
13. Ajayi I, Iken O, Powell RA, Soyannwo O, Namisango E, Mwangi‑Powell F. Palliative care research in Western Africa. Eur J Palliat Care 2014; 21: 45‑7.
14. Onyeka TC. Palliative care in Enugu, Nigeria: Challenges to a new practice. Indian J Palliat Care 2011;17:131‑6.
15. World Health Organization. Cancer Pain Relief and Palliative Care: Report of a WHO Expert Committee. WHO Technical Report Series 804. Geneva: World Health Organization, 1990; 57‑60.
16. Coyle N. Introduction to palliative nursing care. In: Ferrell B, Coyle N, editors. Oxford Textbook of Palliative Nursing. 3rd ed. New York: Oxford University Press, 2010; 3-11.
17. Fineberg IC, Wenger NS, Forrow L. Interdisciplinary education: Evaluation of a palliative care training intervention for pre-professionals. Acad Med 2004;79:769‑76.
18. Bharadwaj P, Vidyasagar MS, Kakria A, Tanvir Alam UA. Survey of palliative care concepts among medical interns in India. J Palliat Med 2007; 10:654‑7.
19. Stjernswärd J, Foley KM, Ferris FD. The public health strategy for palliative care. J Pain Symptom Manage 2007;33:486‑93.