Microbial profile of infections amongst adult in-patients in selected intensive care units in Port Harcourt: a comparative study
Main Article Content
Abstract
Background: The intensive care unit should maintain a minimal presence of pathogenic organisms that could potentially lead to severe infections, particularly in an environment where numerous procedures and interventions compromise the body's normal mucosal defenses.
Aim: To evaluate the prevalence and distribution of common and clinically relevant microorganisms within selected Intensive Care Units (ICUs) in Port Harcourt, Nigeria.
Methods: A prospective, non-randomized study covering January 2022 to December 2024. The study sites were the intensive care units of three hospitals in Port Harcourt: namely the University of Port Harcourt Teaching Hospital (UPTH), Sterling Specialist Hospital, and Prime Medical Consultants. Clinical specimens, including blood samples, urine specimens, respiratory secretions, wound swabs, and venous catheter tips, were collected and analyzed. Data were analyzed using SPSS version 25.
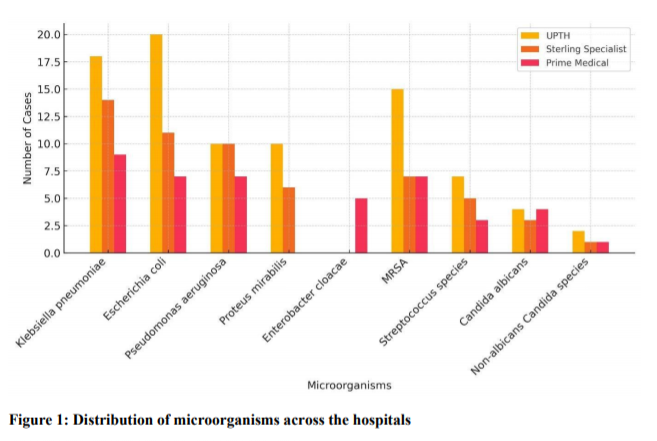
Results: Of the 238 specimens, 186 (78.8%) yielded positive cultures. Gram-negative bacteria (GNB) constituted 68.29% of isolates, followed by Gram-positive bacteria (23.66%) and fungi (8.06%). The most frequently isolated microorganisms were Klebsiella pneumoniae (23.12%), Escherichia coli (19.36%), Pseudomonas aeruginosa (14.52%), Proteus mirabilis (8.60%), and Enterobacter cloacae (2.69%). Among Gram-positive bacteria, methicillin-resistant Staphylococcus aureus (MRSA) accounted for 15.59% of cases, while Streptococcus species constituted 8.07%. Fungal infections accounted for 8.06% and were represented by Candida albicans (5.91%) and non-albicans Candida species (2.15%). UPTH recorded the highest microbial burden, particularly with multidrug-resistant pathogens, compared to the private hospitals.
Conclusion: The study revealed a marked variation in antimicrobial resistance patterns among hospitals, with public hospital demonstrating a notably higher rate of multidrug-resistance in comparison to private hospitals.
Downloads
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
The journal grants the right to make small numbers of printed copies for their personal non-commercial use under Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported License.
References
Vincent J. Nosocomial infections in adult intensive-care units. Lancet 2003; 361(9374): 2068–2077.
Erlandsson CM, Hanberger H, Eliasson I, Hoffmann M, Isaksson B, Lindgren S, et al. Surveillance of antibiotic resistance in ICUs in southeastern Sweden. Acta Anaesthesiol Scand 1999; 43(8): 815–820.
Asensio A, Oliver A, Gonzalez-Diego P, Baquero F, Perez-Diaz JC, Ros P, et al. Outbreak of a multiresistant Klebsiella pneumoniae strain in an intensive care unit: antibiotic use as a risk factor for 4.
Nwadike VU, Ojide CK, Kalu EI. Multidrug resistant Acinetobacter infection and their antimicrobial susceptibility pattern in a Nigerian tertiary hospital ICU. Afr J Infect Dis 2014;8(1):14-18.
Kesah C, Ben Redjeb S, Odugbemi TO, Boye CS, Dosso M, Ndinya Achola JO, et al. Prevalence of methicillin-resistant Staphylococcus aureus in eight African hospitals and Malta. Clin Microbiol Infect 2003; 9(2):153–156.
Morgan GE, Mikhail MS, Murray MJ. Critical care. In: Morgan GE, Mikhail MS, Murray MJ (eds). Clinical anesthesiology, 4th edn. New York: McGraw-Hill Companies Inc., 2006;1050–1051.
Lockhart SR, Abramson MA, Beekmann SE, Gallagher G, Riedel S, Diekema DJ, et al. Antimicrobial resistance among Gram-negative bacilli causing infections in intensive care unit patients in the United States between 1993 and 2004. J Clin Microbiol 2007; 45(10):3352–3359.
American Thoracic Society & Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med 2005; 171(4): 388–416.
Coffin SE, Klompas M, Classen D, Arias KM, Podgorny K, Anderson DJ, et al. Strategies to prevent ventilator-associated pneumonia in acute care hospitals. Infect Control Hosp Epidemiol 2008; 29 Suppl 1: S31–S40.
De Waele JJ, Ravyts M, Depuydt P, Blot SI, Decruyenaere J, Vogelaers D. De-escalation after empirical meropenem treatment in the intensive care unit: fiction or reality? J Crit Care 2010; 25(4): 641–646.
Vincent JL, Rello J, Marshall J, Silva E, Anzueto A, Martin CD, et al. International study of the prevalence and outcomes of infection in intensive care units. JAMA 2009; 302(21): 2323–2329.