Intrathecal versus epidural morphine for analgesia following excisional haemorrhoidectomy: a comparative analysis
Main Article Content
Abstract
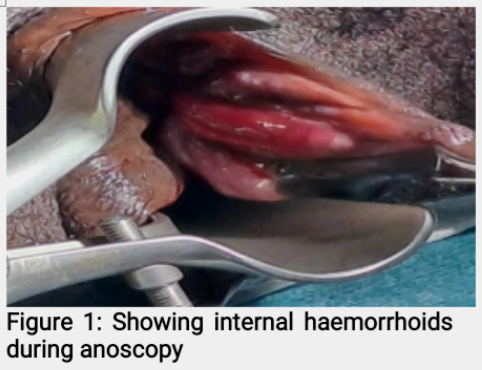
Background: Postoperative pain remains a significant concern in open excisional haemorrhoidectomy, especially for patients with third- and fourth-degree haemorrhoids, which are often associated with severe pain, bleeding, and other debilitating symptoms. Poorly managed postoperative pain adversely affects recovery.
Aim: To compare postoperative pain scores using the Visual Analogue Scale (VAS) after the administration of intrathecal morphine versus epidural morphine, both combined with intravenous paracetamol and rectal diclofenac suppository, for pain management following open excisional haemorrhoidectomy.
Methods: A prospective, randomized controlled study was conducted at the University of Port Harcourt Teaching Hospital (UPTH) over 4years on adult patients with third- or fourth-degree haemorrhoids, for open haemorrhoidectomy. The differences between the two groups were measured using Student t-test and Chi-squared test and were considered statistically significant if p< 0.05.
Results: A total of sixty-six patients completed the study: 30 patients in Group A (intrathecal morphine) and 36 in Group B (epidural morphine). The mean time to a VAS score ≥ 5 cm was significantly shorter in Group A (8.3 ± 4 hours) compared to Group B (24 ± 6.8 hours), with a p-value of 0.0001. Patient satisfaction was reported by 78% of patients in Group A and by all patients (100%) in Group B (p < 0.01).
Conclusion: Epidural morphine, in combination with intravenous paracetamol and rectal suppository, provided superior postoperative pain relief following haemorrhoidectomy and facilitated earlier ambulation compared to intrathecal morphine.
Downloads
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
The journal grants the right to make small numbers of printed copies for their personal non-commercial use under Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported License.
References
Behar M, Magora F, Olshwang D, Davidson JT. Epidural morphine and the treatment of pain. Lancet 1979;1(8115):527-529.
Shapiro LA, Hoffman S, Jedeikir R, Kaplan R. Single-injection epidural anaesthesia with bupivacaine and morphine for prostatectomy. Anesth Analg 1981;60(11):818-820.
Kuo RJ. Epidural morphine for post-haemorrhoidectomy Analgesia. Dis Colon Rectum 1984;27(8):529-530.
Ho YH, Seow-Choen F, Tan M, Leong AF. Randomized controlled trial of open and closed haemorrhoidectomy. Br J Surg 1997;84(9):1729-1730.
Ibrahim S, Tsang C, Lee YL, Eu KW, Seow-Choen F. Prospective, randomized trial comparing pain and complications between diathermy and scissors for closed hemorrhoidectomy. Dis Colon Rectum 1998;41(11):1418-1420.
Brunat G, Pouzeratte Y, Mann C, Didelot JM, Eledjam JJ. Posterior perineal block with ropivacaine 0.75% for pain control during and after hemorrhoidectomy. Reg Anesth Pain Med 2003;28(3):228-232.
Arroyo A, Perez F, Miranda E, Serrano P, Candela F, Lacueva J, et al. Open versus closed day-case haemorrhoidectomy: Is there any difference? Results of a prospective randomized study. Int J Colorectal Dis 2004;19(4):370-373.
Gehling M, Tryba M. Risks and side effects of intrathecal morphine combined with spinal anaesthesia: a meta-analysis. Anaesthesia 2009;64(6):643-651.
Alatise OI, Agbakwuru AE, Takure AO, Akinkuolie AA. Open haemorrhoidectomy under local anaesthesia for symptomatic haemorrhoids: our experience from Nigeria. Arab J Gastroenterol 2011;12(2):99-102.
Lohsiriwat V. Hemorrhoids: from basic pathophysiology to clinical management. World J Gastroenterol 2012;18(17):2009-2017.
Misauno MA, Usman BD, Nnadozie UU, Obiano SK. Experience with rubber band ligation of hemorrhoids in Northern Nigeria. Niger Med J 2013;54(4):258–260.
Kim BC. Spinal block anaesthesia with morphine in a haemorrhoidectomy. Ann Coloproctol 2014;30(3):107-108.
Shaikh AR, Dalwani AG, Sushel C, Halepoto A. Diathermy haemorrhoidectomy: under local Anaesthesia. Professional Med J 2016;23(8):948-952.
Bhatti MI, Sajid MS, Baig MK. Milligan–Morgan (open) versus Ferguson haemorrhoidectomy (closed): a systematic review and meta-analysis of published randomized, controlled trials. World J Surg 2016;40(6):1509-1519.
Akindiose C, Alatise OI, Arowolo OA, Agbakwuru AE. Evaluation of two injection sclerosants in the treatment of symptomatic haemorrhoids in Nigerians. Niger Postgrad Med J 2016;23(3):110–115.
Ray-Offor E, Amadi S. Haemorrhoidal disease; predilection sites, pattern of presentation, and treatment. Ann Afr Med 2019;18(1):12-16.
Gallo G, Martellucci J, Sturiale A, Clerico G, Milito G, Marino F, et al. Consensus statement of the Italian Society of Colorectal Surgery (SICCR): management and treatment of hemorrhoidal disease. Tech Coloproctol 2020;24(2):145-164.
Godeberge P, Sheikh P, Zagriadskiĭ E, Lohsiriwat V, Montaño AJ, Košorok P, et al. Hemorrhoidal disease and chronic venous insufficiency: concomitance or coincidence; results of the CHORUS study (Chronic venous and Hemorrhoidal diseases evaluation and Scientific research). J Gastroenterol Hepatol 2020;35(4):577-585.
Ng KS, Holzgang M, Young C. Still a case of ‘no pain, no gain’? An updated and critical review of the pathogenesis, diagnosis and management options for haemorrhoids in 2020. Ann Coloproctol 2020;36(3):133-147.
Srivastav Y, Prajapati A, Kumar M. Review of haemorrhoids, including quality of life (QOL) and associated contemporary treatments. World J Pharm Res 2023;12(17):283-311.
Amanor-Boadu SD. Assessment of minidose intrathecal morphine for analgesia after haemorrhoidectomy. West Afr J Med 1992;11(2):146-149.