Assessment of medical students’ perception of anatomical pathology teaching methods
Main Article Content
Abstract
Background: Anatomical pathology is an essential component of medical training in the 4th year of medical school and the learning process may be impacted by the effectiveness of delivery methods. This study aimed to assess the perception of medical students on the teaching methods in anatomical pathology.
Methods: A descriptive cross-sectional survey was conducted between January 2024 and January 2025 among medical students across four universities in Southern Nigeria: University of Port Harcourt, Bayelsa Medical University, Gregory University, and Niger Delta University. A structured questionnaire was used to collect data on attendance, preferences, and perceptions of different teaching methods. Responses were entered into Microsoft Excel and analysed in SPSS, applying descriptive statistics such as frequencies and percentages. Results were presented in tables and figures for clarity.
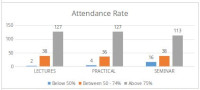
Results: A total of 215 students from four the medical schools responded to this study. The majority were in their 5th year of study. Lectures were the preferred teaching method (65.6%), followed by practical demonstrations (26%) and seminar (8.4%). Students rated the quality of pathology lectures as predominantly good. All the practical demonstration tools were said to make Anatomical pathology more understandable. Among interactive study methods, group discussion was the most preferred.
Conclusion: This study revealed a strong preference among medical students for lectures, practical sessions, as well as group discussions in learning Anatomical Pathology. These findings highlight the need for educators and medical education college boards to integrate and strengthen these interactive and hands-on teaching approaches within the anatomical pathology curriculum.
Downloads
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
The journal grants the right to make small numbers of printed copies for their personal non-commercial use under Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported License.
References
1. Kumar V, Abbas AK, Aster JC. Cellular responses to stress and toxic insults: adaptation, injury, and death. In: Kumar V, Abbas AK, Aster JC, editors. Robbins and Cotran Pathologic basis of disease, 10th edition. Philadelphia: Elsevier, 2020;33‑55.
2. Strayer DS, Rubin E. Cell injury . In: Rubin R, Strayer DS, editors. Rubin’s pathology: clinicopathologic foundations of medicine, 6th edition. Philadelphia: Lippincott Williams and Wilkins, 2012; 5-41.
3. Vijayan P, Ponniah A. A survey study based on undergraduate medical students’ feedback regarding pathology and the teaching-learning methodologies employed. Trop J Pathol Microbiol 2017;3(2):149–154.
4. Kerby J, Shukur ZN, Shalhoub J. The relationships between learning outcomes and methods of teaching anatomy as perceived by medical students. Clin Anat 2011;24(4):489–497.
5. Fernández-Rodríguez CA, Arenas-Fenollar MC, Lacruz-Pérez I, Tárraga-Mínguez R. Teaching methods in medical education: an analysis of the assessments and preferences of students. Sustainability 2023;15(11):9044.
6. Ware AD, Murdock T, Voltaggio L, Windon AL, Troncoso JC, Hruban RH, et al. The “race” toward diversity, inclusion, and equity in pathology: the Johns Hopkins experience. . Acad Pathol 2019;6:2374289519873104.
7. Lee LMJ, Goldman HM, Hortsch M. The virtual microscopy database sharing digital microscope images for research and education. Anat Sci Educ 2018;11(5):510-515.
8. Harden RM, Crosby J. AMEE Guide No 20: The good teacher is more than a lecturer—the twelve roles of the teacher. Med Teach 2000;22(4):334–347.
9. Barrows HS. Problem-based learning in medicine and beyond: a brief overview. New Dir Teach Learn 1996;(68):3–12.
10. Chiu BK, Solez K, Sergi CM. Digital pathology for e-learning and digital education – a review. J Inform Technol Appl Educ 2014;3(4):164 - 168..
11. Haidet P, Kubitz K, McCormack WT. Analysis of the team-based learning literature: TBL comes of age. J Excell Coll Teach 2014;25(3–4):303–333.
12. Patterson JS, Stickle JE, Thomas JS, Scott MA. An integrative and case-based approach to the teaching of general and systemic pathology. J Vet Med Educ 2007;34(4):409–415.
13. Rahman N, Ferdousi S, Hoq N, Amin R, Kabir J. Evaluation of objective structured practical examination and traditional practical examination. Mymensingh Med J 2007;16(1):7–11.
14. Entwistle N, Tait H. Approaches to learning, evaluations of teaching, and preferences for contrasting academic environments. High Educ 1990;19(2):169–194.
15. Wimpenny K. Student engagement in higher education: theoretical perspectives and practical approaches for diverse populations: second edition. Educ Psychol 2014;36(5):1044–1046.
16. Dewey J. Experience and education. New York: Macmillan, 1938.
17. Ellaway R, Masters K. AMEE Guide 32: e-Learning in medical education Part 1: Learning, teaching and assessment. Med Teach 2008;30(5):455-473.
18. Cook DA, Levinson AJ, Garside S, Dupras DM, Erwin PJ, Montori VM. Instructional design variations in internet-based learning for health professions education: a systematic review and meta-analysis. Acad Med 2010;85(5):909–922.
19. Pallant J. SPSS survival manual: a step-by-step guide to data analysis using IBM SPSS, 7th ed. New York: Routledge, 2020.
20. Cohen J. Statistical power analysis for the behavioral sciences, 2nd ed. Hillsdale, NJ: Lawrence Erlbaum, 1988.
21. Bhagyalakshmi A, Sridevi D, Dambal AA, Ravibabu K, Chaitanya GL. Effectiveness of seminar as an educational tool among the undergraduate medical students: a study. MRIMS J Health Sci 2020;8(2): 43-46.
22. Kasi Babu A, Vijaya Babu PVSS, Bhagya lakshmi A, Kumar SV. Evaluation of the effectiveness of seminar as an educational tool among the medical post graduate students. Int J Res Med Sci 2016;4(3):877-880.
23. Moore R, Jensen M, Hatch J, Duranczyk I, Staats S, Koch L. Showing up: The importance of class attendance for academic success in introductory science courses. Am Biol Teach 2003;65(5):325–329.
24. Wolff M, Wagner MJ, Poznanski S, Schiller J, Santen S. Not another boring lecture: engaging learners with active learning techniques. J Emerg Med 2015;48(1):85–93.
25. Kahu ER, Picton C, Nelson K. Pathways to engagement: a longitudinal study of the first-year student experience in the educational interface. High Educ 2020;79(4):657–673.
26. Kahu ER. Framing student engagement in higher education. Stud High Educ 2013;38(5):758–773.
27. Picton C, Baik C. Conceptualising student engagement in higher education. Stud Success 2024;15(3):1-9.
28. Singh K, Gaur U, Hall K, Mascoll K, Cohall D, Majumder MA. Teaching anatomy and dissection in an era of social distancing and remote learning. Adv Hum Biol 2020;10(3):90-94.
29. Yusof YA, Taridi NM, Mustapa M, Shaharuddin S, Hamid MW, Shakrin NN. Student‑centred approach in medical education: a review of the teaching‑learning activities and the perceptions of educators on the students engagement and performance at the faculty of medicine and defence health, national defence university of Malaysia. Adv Hum Biol 2022;12(2):101-107.
30. Al Shenawi H, Yaghan R, Almarabheh A, Al Shenawi N. The relationship between attendance and academic performance of undergraduate medical students during surgical clerkship. BMC Med Educ 2021;21(1):396.
31. Subramaniam B, Hande S, Komattil R. Attendance and achievement in medicine: investigating the impact of attendance policies on academic performance of medical students. Ann Med Health Sci Res 2013;3(2):202-205.
32. Freeman S, Eddy SL, McDonough M, Smith MK, Okoroafor N, Jordt H, et al. Active learning increases student performance in science, engineering, and mathematics. Proc Natl Acad Sci U S A 2014;111(23):8410–8415.
33. Theobald EJ, Hill MJ, Tran E, Agrawal S, Arroyo EN, Behling S, et al. Active learning narrows achievement gaps for underrepresented students in undergraduate science, technology, engineering, and math. Proc Natl Acad Sci U S A 2020;117(12):6476–6483.
34. Turney B. Anatomy in a modern medical curriculum. Ann R Coll Surg Engl 2007;89(2):104–107.
35. Moro C, Štromberga Z, Raikos A, Stirling A. The effectiveness of virtual and augmented reality in health sciences and medical anatomy. Anat Sci Educ 2017;10(6):549–559.
36. Kolb DA. Experiential learning: Experience as the source of learning and development. Englewood Cliffs, NJ: Prentice Hall, 2014.
37. Panusch P, Heide S, Lessig R, Richter C, Stiller D, Medenwald D, et al. Evaluation of occupational factors influencing the experience of an autopsy demonstration. Rechtsmedizin 2023;33(6):464–470.
38. Steinert Y, Snell LS. Interactive lecturing: strategies for increasing participation in large group presentations. Med Teach 1999;21(1):37–42.