Evaluation of the psychological distress experienced by spouses of women undergoing anaesthesia for caesarean section
Main Article Content
Abstract
Background: Caesarean section (CS) could serve a challenging situation to spouses and family of women, more so as these women are meant to undergo anaesthesia. Little evidence exists with regard to the psychological impact of this on these families.
Aim: The study was aimed to evaluate psychological distress among spouses of women undergoing anaesthesia for CS and also to identify the coping strategies used by the participants.
Methods: Ninety-one husbands of women undergoing anaesthesia for CS were consecutively recruited. They were given a self-administered study protocol consisting of sociodemographic questionnaire, General Health Questionnaire (GHQ-12) and the Brief Cope Inventory. P < 0.05 was considered statistically significant.
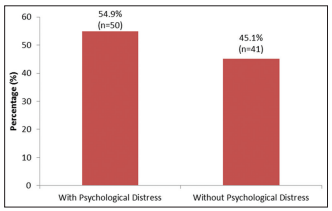
Results: Fifty participants (54.9%) were found to have psychological distress (GHQ of 3 and above). Psychological distress was significantly more amongst younger participants (20–39 years’ age group: 100% and 30–39 years’ age group: 57.4%, P < 0.05). A significantly higher proportion (72.4%) of participants were unemployed, whereas those without previous experience of birth (85.0%) had psychological distress(P < 0.05). However, employment status(OR=3.5; 95%CI; 1.24-9.98) and previous birth experience [(OR 95% CI, 6.3 (1.59 - 24.78)] predicted the outcome of psychological distress among the participants on multivariate analysis. The mean scores on the coping subscales of substance use, positive reframing, planning and self-blame were significantly higher among those with psychological distress in comparison to those without psychological distress (P < 0.05).
Conclusion: The prevalence of psychological distress is high among the husbands of women undergoing anaesthesia for CS. Substance use, positive reframing, planning and self-blame were more observed among those with psychological distress.
Downloads
Article Details
The journal grants the right to make small numbers of printed copies for their personal non-commercial use under Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported License.
References
1. Kurtz ME, Kurtz JC, Given CW, Given B. Relationship of caregiver reactions and depression to cancer patients’ symptoms, functional states and depression – A longitudinal view. Soc Sci Med 1995;40:837‑46.
2. Kainu JP, Sarvela J, Tiippana E, Halmesmäki E, Korttila KT. Persistent pain after caesarean section and vaginal birth: A cohort study. Int J Obstet Anesth 2010;19:4‑9.
3. Ukpong DI, Owolabi AT. Postpartum emotional distress: A controlled study of Nigerian women after caesarean childbirth. J Obstet Gynaecol
2006;26:127‑9.
4. Maclean L, McDermott M, May C. Method of delivery and subjective distress: Women’s emotional responses to childbirth practices. J Reprod
Infant Psychol 2000;18:153‑62.
5. Beutel M, Willner H, Deckardt R, Von Rad M, Weiner H. Similarities and differences in couples’ grief reactions following a miscarriage: Results from a longitudinal study. J Psychosom Res 1996;40:245‑53.
6. Afridi MI, Mashhood A. Anxiety, depression and stress among the husbands of obstetric cases at Karachi. J Pak Med Assoc 1999;49:265‑8.
7. Masjedi M, Ghorbani M, Managheb I, Fattahi Z, Dehghanpisheh L, Salari M, et al. Evaluation of anxiety and fear about anesthesia in adults undergoing surgery under general anesthesia. Acta Anaesth Belg 2017;68:25‑9.
8. Mavridou P, Dimitriou V, Manataki A, Arnaoutoglou E, Papadopoulos G. Patient’s anxiety and fear of anesthesia: Effect of gender, age, education, and previous experience of anesthesia. Asurvey of 400 patients. J Anesth 2013;27:104‑8.
9. Gruenais ME, Ouattara F. The price of childbirth. Pregnancy management in sub‑Saharan Africa. Families and Health: The Look of the Social Sciences. Rennes, France: Presses of the School of Higher Studies in Public Health, 2010.
10. Ouattara F, Bationo F, Gruenais ME. No mother without a “husband”. The need for marriage in health care facilities in Ouagadougou
(Burkina Faso). Autrepart 2009;52:79‑92.
11. Onoka CA, Onwujekwe OE, Hanson K, Uzochukwu BS. Examining catastrophic health expenditures at variable thresholds using household consumption expenditure diaries. Trop Med Int Health 2011;16:1334‑41.
12. Onwujekwe O, Hanson K, Uzochukwu B, Ichoku H, Ike E, Onwughalu B. Are malaria treatment expenditures catastrophic to different socio‑economic and geographic groups and how do they cope with payment? A study in Southeast Nigeria. Trop Med Int Health 2010;15:18‑25.
13. Mato CN, Tobin M. Out‑of‑pocket health expenditure: A preliminary survey of impact on households of patients in the intensive care unit of
a tertiary hospital in Nigeria. Afr J Anaesth Intensive Care 2009;9:1‑4.
14. Deb P, Gallo WT, Ayyagari P, Fletcher JM, Sindelar JL. The effect of job loss on overweight and drinking. J Health Econ 2011;30:317‑27.
15. Murphy G, Athanasou J. The effect of unemployment on mental health. J Occup Organ Psychol 1999;72:83‑99.
16. Bambra C. Yesterday once more? Unemployment and health in the 21st century. J Epidemiol Community Health 2010;64:213‑5.
17. Plantin L, Olukoya AA, Ny P. Positive health outcomes of fathers’ involvement in pregnancy and childbirth paternal support. A scope study literature review. Fathering 2011;9:87‑102.
18. Gottfredsdóttir H, Sandall J, Björnsdóttir K. ‘This is just what you do when you are pregnant’: A qualitative study of prospective parents in Iceland who accept nuchal translucency screening. Midwifery 2009;25:711‑20.
19. Nelson K. Event representations, narrative development and internal working models. Attach Hum Dev 1999;1:239‑52.
20. Donovan J. The process of analysis during a grounded theory study of men during their partners’ pregnancies. J Adv Nurs 1995;21:708‑15.
21. Brammer LM. Coping with life transitions. Int J Adv Counsell 1992;15:239‑53.