Abruptio placentae: Epidemiology and pregnancy outcome in a low‑resource setting
Main Article Content
Abstract
Background: Abruptio placentae are a life-threatening obstetric emergency associated with high maternal, foetal and neonatal morbidity and mortality.
Aim: The aim of this study is to determine the modes of presentation, management and pregnancy outcome of pregnancies complicated by abruptio placentae at a tertiary health facility.
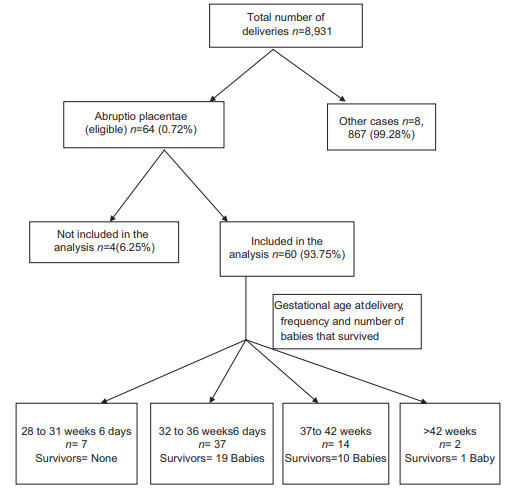
Methods: A descriptive study (retrospective) of women managed for abruptio placentae over a period of 3 years. The inclusion criteria were diagnosis of abruptio placentae (clinical or radiological), delivery at the study site and availability of the case files for review. Exclusion criteria included patients with other conditions except abruptio placentae, delivery at other facilities or failure to retrieve the case files. Data collection was from the case files of participants, and the results were represented in tables.
Results: Out of 8,931 deliveries during study , 64 had for abruptio placentae (prevalence 0.72% or 7.2/1000); however, 60 satisfied the inclusion criteria and were included in subsequent analysis. Twenty (33.3%) were above 35 years old, 14 (23.3%) were grandmultipara and the most common risk factor was hypertensive disorders (26; 43.3%). Thirty (50.0%) presented with vaginal bleeding, retroplacental clot was present at delivery in 27 (45.0%), 37 (61.7%) had emergency abdominal delivery, 51 (85.0%) had anaemia at presentation while 37 (61.6%) had blood transfusion. Forty-four (73.4%) were preterm (mean gestational age 35 ± 2.9 weeks) and neonatal survival was 50.0%; among survivors, 25 (83.3%) required neonatal intensive care due to perinatal asphyxia. Perinatal mortality was 50% (500/1,000), but no maternal death among study participants.
Conclusion: Abruptio placentae remain a potential cause of maternal, foetal and neonatal complications; however, emergency caesarean delivery appears to improve neonatal survival in complicated cases with live foetuses.
Downloads
Article Details
The journal grants the right to make small numbers of printed copies for their personal non-commercial use under Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported License.
References
1. Sarah A. Third‑trimester vaginal bleeding. In: Decherney AH, Nathan L, Roman A, Lauren N, editors. Current Diagnosis and Treatment: Obstetrics and Gynaecology. 11th ed. New York: McGraw Hill, 2013; 310‑3.
2. Hall DR. Abruptio placentae and disseminated intravascular coagulopathy. Semin Perinatol 2009;33:189‑95.
3. Takeda A, Imoto S, Nakamura H. Abruptio placentae in subsequent pregnancy after conservative management of hemorrhagic cesarean
scar pregnancy by transcatheter arterial chemoembolization. Clin Med Insights Case Rep 2013;6:137‑40.
4. Bibi S, Memon A, Sheikh JM, Qureshi AH. Severe acute maternal morbidity and intensive care in a public sector university hospital of
Pakistan. J Ayub Med Coll Abbottabad 2008;20:109‑12.
5. Kwawukume EY. Antepartum haemorrhage. In: Kwawukume EY, Emuveyan EE, editors. Comprehensive Obstetrics in the Tropics. 1st ed. Accra: Asante, Hittscher, 2002; 145‑50.
6. Ozumba BC. Abruptio placentae at the university of Nigeria teaching hospital, Enugu: A 3‑year study. Aust N Z J Obstet Gynaecol 1989; 29:117‑20.
7. Kay HH. Placenta praevia and abruptio. In: Gibbs RS, editor. Danforth’s Obstetrics and Gynaecology. 10th ed. Philadelphia: Lippincott Williams & Wilkins, 2008; 387‑99.
8. Olayemi O, Bello FA, Aimakhu CO, Obajimi GO, Adekunle AO. Male participation in pregnancy and delivery in Nigeria: A survey of antenatal attendees. J Biosoc Sci 2009;41:493‑503.
9. Oyelese Y, Ananth CV. Placental abruption. Obstet Gynecol 2006;108:1005‑16.
10. SarwarI, Abbasi Au, Islam A. Abruptio placentae and its complications at Ayub teaching hospital Abbottabad. J Ayub Med Coll Abbottabad
2006;18:27‑31.
11. Macheku GS, Philemon RN, Oneko O, Mlay PS, Masenga G, Obure J, et al. Frequency, risk factors and feto‑maternal outcomes of abruptio
placentae in Northern Tanzania: A registry‑based retrospective cohort study. BMC Pregnancy Childbirth 2015;15:242.
12. Nkwabong E, Tiomela Goula G. Placenta abruption surface and perinatal outcome. J Matern Fetal Neonatal Med 2017;30:1456‑9.
13. Hossain N, Khan N, Sultana SS, Khan N. Abruptio placenta and adverse pregnancy outcome. J Pak Med Assoc 2010;60:443‑6.
14. Tikkanen M, Nuutila M, Hiilesmaa V, Paavonen J, Ylikorkala O. Clinical presentation and risk factors of placental abruption. Acta Obstet
Gynecol Scand 2006;85:700‑5.
15. Tikkanen M. Placental abruption: Epidemiology, risk factors and consequences. Acta Obstet Gynecol Scand 2011;90:140‑9.
16. Sheiner E, Shoham‑VardiI, HadarA, Hallak M, Hackmon R, Mazor M, et al. Incidence, obstetric risk factors and pregnancy outcome of
preterm placental abruption: A retrospective analysis. J Matern Fetal Neonatal Med 2002;11:34‑9.
17. Tikkanen M. Etiology, clinical manifestations, and prediction of placental abruption. Acta Obstet Gynecol Scand 2010;89:732‑40.
18. Pariente G, WiznitzerA, Sergienko R, Mazor M, Holcberg G, SheinerE, et al. Placental abruption: Critical analysis of risk factors and perinatal
outcomes. J Matern Fetal Neonatal Med 2011;24:698‑702.
19. Witlin AG, Sibai BM. Perinatal and maternal outcome following abruptio placentae. Hypertens Pregnancy 2001;20:195‑203.
20. Jahić M, Jahić E, Nurkić M, Nurkić J. Hypertension in pregnancy. Med Arh 2008;62:169‑71.
21. Goodnough LT, Daniels K, Wong AE, Viele M, Fontaine MF, Butwick AJ, et al. How we treat: Transfusion medicine support of obstetric services. Transfusion 2011;51:2540‑8.