Ototoxicity: Scope and pattern in a tertiary hospital in Port Harcourt, Nigeria
Main Article Content
Abstract
Background: Ototoxicity is a common cause of avoidable hearing loss in our environment. It is also an important factor of public health importance in developing countries. The aim of this study is to examine the pattern, note the prevalence and highlight the common medications implicated in ototoxicity in our environment.
Methods: This study is a 6-year retrospective review of patients diagnosed with ototoxicity that were managed at the otorhinolaryngology clinic from January 2011 to December 2016. The patients’ case files and the clinical registries were the source of data. The data extracted for analysis were demographics, type of medication used, route of administration, duration, otologic symptoms, time of presentation and pure-tone audiometric findings. Data were analysed using SPSS software version 20.
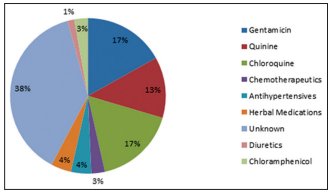
Results: One hundred and thirty-six patients with ototoxicity were seen within the 6-year period, of which 71 had complete medical records and these were analysed. There were 37 males (52.1%) and 34 females (47.9%), giving a ratio of 1:1. The most common age group affected was 28–38 years. Unknown or unidentified medications (38%) were the most common cause of ototoxicity; among the known drugs, injection gentamicin (17%) and chloroquine (17%) were the most common implicated drugs, followed by quinine (12.7%). All the patients presented with hearing loss. Tinnitus was seen in 83.1%, whereas 22.5% had vertigo. Majority (56.3%) of the patients had severe-to-profound sensorineural hearing loss. There were more bilateral (80.3%) than unilateral (19.7%) cases. Majority (63.3%) of the patients presented after 2 weeks of the onset of symptoms.
Conclusion: Ototoxicity is still prevalent in our environment, with chloroquine and gentamicin being the most commonly implicated drugs. Most of the patients were found to have bilateral severe-to-profound sensorineural hearing loss.
Downloads
Article Details
The journal grants the right to make small numbers of printed copies for their personal non-commercial use under Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported License.
References
1. Smith AW. The World Health Organisation and the prevention of deafness and hearing impairment caused by noise. Noise Health 1998; 1:6‑12.
2. Fausti SA, Henry JA, Schaffer HI, Olson DJ, Frey RH, McDonald WJ, et al. High‑frequency audiometric monitoring for early detection of
aminoglycoside ototoxicity. J Infect Dis 1992;165:1026‑32.
3. Petersen LO, Rogers C. Aminoglycoside induced hearing deficits – A review of cochlear ototoxicity. South Afr Fam Pract 2015;57:77‑82.
4. Stelmachowicz PG, Pittman AL, Hoover BM, Lewis DE, Moeller MP. The importance of high‑frequency audibility in the speech and language development of children with hearing loss. Arch Otolaryngol Head Neck Surg 2004;130:556‑62.
5. World Health Organization. Programme for the Prevention of Deafness and Hearing Impairment. Report of an Informal Consultation on Strategies for Prevention of Hearing Impairments from Ototoxic Drugs, WHO/PDH/95.2. Geneva: World Health Organization; 1995. Available from: http://www.who.int/iris/handle/10665/62065. [Last accessed on 2012 Jun 16].
6. BuszmanE, WrzenisckD, MatusinkiB. Ototoxic drugs. Aminoglycoside antibiotics. Wiad Lek 2003;56:254‑9.
7. Hayes DM, CvitkovicE, Golbey RB, ScheinerE, Helson L, Krakoff IH, et al. High dose cis‑platinum diammine dichloride: Amelioration of renal toxicity by mannitol diuresis. Cancer 1977;39:1372‑81.
8. Jung TT, Rhee CK, Lee CS, Park YS, Choi DC. Ototoxicity of salicylate, nonsteroidal antiinflammatory drugs, and quinine. Otolaryngol Clin North Am 1993;26:791‑810.
9. Rybak LP, Ramkumar V. Ototoxicity. Kidney Int 2007;72:931‑5.
10. Lee CS, Heinrich J, Jung TT. Quinine induced ototoxicity: Alterations in cochlear blood flow. Otolaryngol Head Neck Surg 1992;107:233.
11. Schacht J, Talaska AE, Rybak LP. Cisplatin and aminoglycoside antibiotics: Hearing loss and its prevention. Anat Rec (Hoboken) 2012; 295: 1837‑50.
12. Bokemeyer C, Berger CC, Hartmann JT, Kollmannsberger C, Schmoll HJ, Kuczyk MA, et al. Analysis of risk factors for cisplatin‑induced ototoxicity in patients with testicular cancer. Br J Cancer 1998;77:1355‑62.
13. Kokong DD, Bakari A, Ahmad BM. Ototoxicity in Nigeria: Why it persists. Ear Nose Throat J 2014;93:256‑64.
14. Salisu AD, Hasheem MG. Pattern of ototoxicity in a Nigerian teaching hospital. Niger J Med 2010;19:320‑3.
15. Obasikene G, Adobamen P, Okundia P, Ogusi FO. Prevalence of ototoxicity in university of Benin teaching hospital, Benin city: A 5‑year
review. Niger J Clin Pract 2012;15:453‑7.
16. Maude RJ, Dondorp AM, Faiz MA, Yunus EB, Samad R, Hossain A, et al. Malaria in Southeast Bangladesh: A descriptive study. Bangladesh
Med Res Counc Bull 2008;34:87‑9.
17. Zhao SZ, Mackenzie IJ. Deafness: Malaria as a forgotten cause. Ann Trop Paediatr 2011;31:1‑10.
18. Dunmade AD, Segun‑Busari S, Olajide TG, Ologe FE. Profound bilateral sensorineural hearing loss in Nigerian children: Any shift in etiology? J Deaf Stud Deaf Educ 2007;12:112‑8.
19. Ogisi FO. Chloramphenicol induced hearing loss. Niger J Surg Res 2001;3:75‑80.
20. Mukherjee DK, Mukherjee K. Ototoxicity of commonly used pharmaceutical preparations. Niger Med J 1979;9:52‑7.
21. Bisht M, Bist SS. Ototoxicity: The hidden menace. Indian J Otolaryngol Head Neck Surg 2011;63:255‑9.
22. Duggal P, Sarkar M. Audiologic monitoring of multi‑drug resistant tuberculosis patients on aminoglycoside treatment with long term
follow‑up. BMC Ear Nose Throat Disord 2007;7:5.
23. Kharkheli E, Kevanishvili Z, Maglakelidze T, Davitashvili O, Schacht J. Does Vitamin E prevent gentamicin‑induced ototoxicity? Georgian
Med News 2007;146:14‑7.
24. Indudharan R, Valuyeetham KA, Raju SS. Role of glucocorticoids in ototopical antibiotic‑steroid preparations in the treatment of chronic
suppurative otitis media. Arch Med Res 2005;36:154‑8.
25. Harris T, Peer S, Fagan JJ. Audiological monitoring for ototoxic tuberculosis, human immunodeficiency virus and cancer therapies in a developing world setting. J Laryngol Otol 2012;126:548‑51.
26. Grohskopf LA, Huskins WC, Sinkowitz‑Cochran RL, Levine GL, Goldmann DA, Jarvis WR, et al. Use of antimicrobial agents in United States neonatal and pediatric intensive care patients. Pediatr Infect Dis J 2005;24:766‑73.
27. Schacht J, Hawkins JE. Sketches of otohistory. Part 11: Ototoxicity: Drug‑induced hearing loss. Audiol Neurootol 2006;11:1‑6.
28. Olusanya BO, Newton VE. Global burden of childhood hearing impairment and disease control priorities for developing countries. Lancet 2007;369:1314‑7.
29. American Speech‑Language‑Hearing Association. Audiologic management of individuals receiving cochleotoxic drug therapy. Guidelines for audiologic management of individuals receiving cochleotoxic drug therapy. ASHA 1994;36 (Suppl 12):11‑9. Availabe from: www.asha.org. [Last accessed on 2017 Jun 07].