Two nights in one day: A case report of paraganglioma in sickle cell disease and a review of the literature
Main Article Content
Abstract
Background: Sickle cell disease (SCD) is a chronic lifelong disease seen typically in Sub-Saharan Africans, the Mediterranean region and parts of Asia. The condition may be associated with other clinical entities.
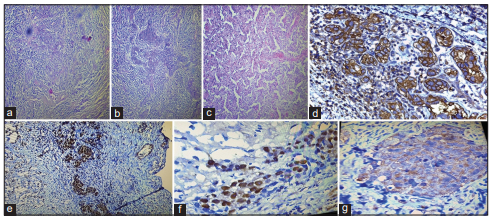
Aim of Presentation: We present a case of malignant variant of paraganglioma in a 34-year-old SCD patient to highlight the fact that some very rare clinical entities may be found in this category of patients.
Case Report: Miss B.O. was a 34-year-old SCD patient who presented with features of an intra-abdominal mass. Incisional biopsy done from a mass arising from the left adrenal gland confirmed a malignant variant of paraganglioma. Post-exploratory laparotomy, the patient’s clinical state deteriorated and she died 25 days after surgery.
Conclusion: Malignant variant of a paraganglioma, a very rare clinical condition, may be found in SCD patients.
Downloads
Article Details
The journal grants the right to make small numbers of printed copies for their personal non-commercial use under Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported License.
References
1. Rees DC, Williams TN, Gladwin MT. Sickle‑cell disease. Lancet 2010;376:2018‑31.
2. National Health Service. NHS Choices. Bristol, UK: IOP Publishing. Available from: http://www.nhs.uk/conditions/Sickle‑cell‑anaemia/Pages/Introduction.aspx. [Last assessed on 2019 Apr 16].
3. Goldin AG, Kelty KC, Beard MF. Sickle cell anemia terminating in acute myeloblastic leukemia. Ann Intern Med 1953;39:920‑8.
4. Samal GC. Sickle cell anemia with acute myeloid leukemia – (A case report). Indian Pediatr 1979;16:453‑4.
5. Salmassi S, Currie ET, Bolf EC, Hernandez M, Kasprisin DO. Management of Hodgkin’s disease in a patient with sickle cell anemia. Cancer 1981; 48:252‑4.
6. Paydas S. Sickle cell anemia and hematological neoplasias. Leuk Lymphoma 2002;43:1431‑4.
7. Schultz WH, Ware RE. Malignancy in patients with sickle cell disease. Am J Hematol 2003;74:249‑53.
8. Dawkins FW, Kim KS, Squires RS, Chisholm R, Kark JA, Perlin E, et al. Cancer incidence rate and mortality rate in sickle cell disease patients at
Howard university hospital: 1986‑1995. Am J Hematol 1997;55:188‑92.
9. Labi M, Haponik EF, Welsh RA, Summer WR. Alveolar cell carcinoma complicating sickle cell anemia: A chance occurrence? Am J Hematol 1989; 32:222‑5.
10. Tawfik OW, Moral LA, Richardson WP, Lee KR. Multicentric bilateral renal cell carcinomas and a vascular leiomyoma in a child. Pediatr Pathol
1993;13:289‑98.
11. Shokunbi WA, Campbell OB, Ogunbiyi JO. Malignant haemangioendothelioma of bone in a HbSC disease patient – A case report. Afr J Med Med Sci 1996;25:293‑6.
12. Stricker RB, Linker CA, Crowley TJ, Embury SH. Hematologic malignancy in sickle cell disease: Report of four cases and review of the literature. Am J Hematol 1986;21:223‑30.
13. Seminog OO, Ogunlaja OI, Yeates D, Goldacre MJ. Risk of individual malignant neoplasms in patients with sickle cell disease: English
national record linkage study. J R Soc Med 2016;109:303‑9.
14. Chen H, Sippel RS, O’Dorisio MS, Vinik AI, Lloyd RV, Pacak K, et al. The North American neuroendocrine tumor society consensus guideline for the diagnosis and management of neuroendocrinen tumors: Pheochromocytoma, paraganglioma, and medullary thyroid cancer. Pancreas 2010;39:775‑83.
15. Jansen JC, van den BergR, KuiperA, van der MeyAG, ZwindermanAH, Cornelisse CJ, et al. Estimation of growth rate in patients with head
and neck paragangliomas influences the treatment proposal. Cancer 2000; 88:2811‑6.
16. Granger JK, Houn HY. Head and neck paragangliomas: A clinicopathologic study with DNA flow cytometric analysis. South Med J 1990; 83:1407‑12.
17. Scholz T, Schulz C, Klose S, Lehnert H. Diagnostic management of benign and malignant pheochromocytoma. Exp Clin Endocrinol
Diabetes 2007;115:155‑9.
18. Mannelli M, Castellano M, Schiavi F, Filetti S, Giacchè M, Mori L, et al. Clinically guided genetic screening in a large cohort of Italian patients with pheochromocytomas and/or functional or nonfunctional paragangliomas. J Clin Endocrinol Metab 2009;94:1541‑7.
19. Gimenez‑Roqueplo AP, Dahia PL, Robledo M. An update on the genetics of paraganglioma, pheochromocytoma, and associated hereditary syndromes. Horm Metab Res 2012;44:328‑33.
20. Neumann HP, Bausch B, McWhinney SR, Bender BU, Gimm O, Franke G, et al. Germ‑line mutations in nonsyndromic pheochromocytoma. N Engl J Med 2002;346:1459‑66.
21. Amar L, Bertherat J, Baudin E, Ajzenberg C, Bressac‑de Paillerets B, Chabre O, et al. Genetic testing in pheochromocytoma or functional
paraganglioma. J Clin Oncol 2005;23:8812‑8.
22. Herrick JB. Peculiar elongated and sickle‑shaped red blood corpuscles in a case of severe anaemia. Arch Int Med 1910;6:517‑21.
23. Fleming AF. Haematologic disease. In: Strickland GT, editor. Hunter’s Tropical Medicine and Emerging Infectious Diseases. 8th ed. Philadelphia: W.B. Saunders Company; 2000. p. 1192.
24. Goldacre M, Kurina L, Yeates D, Seagroatt V, Gill L. Use of large medical databases to study associations between diseases. QJM 2000; 93:669‑75.
25. Goldacre MJ, Wotton CJ, Seagroatt V, Yeates D. Cancers and immune related diseases associated with Down’s syndrome: A record linkage
study. Arch Dis Child 2004;89:1014‑7.
26. Turner MR, Goldacre R, Goldacre MJ. Reduced cancer incidence in Huntington’s disease: Record linkage study clue to an evolutionary trade‑off? Clin Genet 2013;83:588‑90.
27. Antwi‑Boasiako C, Frimpong E, Gyan B, Kyei‑Baafour E, Sey F, Dzudzor B, et al. Elevated proangiogenic markers are associated with vascular complications within Ghanaian sickle cell disease patients. Med Sci (Basel) 2018;6. pii: E53.
28. Vamvakas EC, Blajchman MA. Deleterious clinical effects of transfusion‑associated immunomodulation: Fact or fiction? Blood 2001; 97:1180‑95.
29. Snyder RD. The role of deoxynucleoside triphosphate pools in the inhibition of DNA‑excision repair and replication in human cells by
hydroxyurea. Mutat Res 1984;131:163‑72.
30. Li JC, Kaminskas E. Progressive formation of DNA lesions in cultured Ehrlich ascites tumor cells treated with hydroxyurea. Cancer Res 1987; 47:2755‑8.
31. Najean Y, Rain JD. Treatment of polycythemia Vera: Use of 32P alone or in combination with maintenance therapy using hydroxyurea in
461 patients greater than 65 years of age. The french polycythemia study group. Blood 1997;89:2319‑27.
32. Phillips LN, Krishnamurti L, Rytting H, Olson TA. Ovarian sertoli‑leydig tumor after bone marrow transplant for sickle cell disease. Pediatr Blood Cancer 2018;65:e27367.
33. Stricker TP, Kumar V. Neoplasia. In: Kumar V, Abbas AK, Fausto N, Mitchell RN, editors. Robbins Basic Pathology. 8th ed. Philadelphia:
Saunders Elsevier; 2007. p. 516‑22.
34. Sanford DE, Goedegebuure SP, Eberlein TJ. Tumour biology and tumour markers. In: Sabiston Textbook of Surgery: The Biological Basis of Modern Surgical Practice. 20th ed. Philadelphia: Elsevier; 2017. p. 689‑97.
35. Thomas T, Thomas D, French K, Binder AM. Malignancy in patients with sickle cell disease: A single centre observational study. Blood 2016; 128:4867‑71.
36. Wilzén A, Rehammar A, Muth A, Nilsson O, Tešan Tomić T, Wängberg B, et al. Malignant pheochromocytomas/paragangliomas harbor mutations in transport and cell adhesion genes. Int J Cancer 2016; 138:2201‑11.
37. Asa SL, Ezzat S, Mete O. The diagnosis and clinical significance of paragangliomas in unusual locations. J Clin Med 2018;7. pii: E280.