Evaluation of antimalarial drugs usage according to WHO prescribing indicators in a tertiary health facility in Maiduguri, Northeastern Nigeria
Main Article Content
Abstract
Background: The high morbidity and mortality associated with malaria especially in sub-Saharan Africa such as Nigeria calls for prompt preventive and curative measures including adherence to standard treatment guideline.
Aim: To assess the level of adherence with the five defined WHO prescribing key indicators.
Methods: This was a retrospective evaluation of the performance of antimalarial drugs prescribing practice among clinicians from January to December 2014. It was done through a set of drug prescribing indicators developed by WHO and the International Network of Rational Use of Drugs (INRUD).
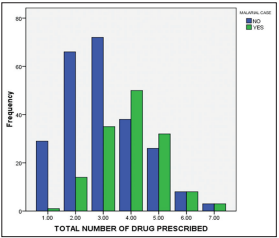
Results: Of the 385 patients prescription randomly generated from the record of 12,477 patients in this descriptive study, a total of 143 (37.1%) had antimalarial prescription(s) with no gender variation. The evaluation of the studied antimalarial drug prescriptions through defined WHO prescribing indicators revealed an average number of drugs per encounter of 3.9, with 37.4% of the prescriptions written in generic names. All the antimalarial drugs were prescribed from the National Drug Formulary, with injectable form constituting 4.7%.
Conclusion: This study shows suboptimal compliance with WHO prescribing indicators with respect to average number of antimalarial per encounter and prescription in generic names. The proportion of antimalarials prescription in injectable form falls within the WHO acceptable limit of ≤10%. All antimalarial drug prescriptions in this study were from essential drug list. We, therefore, recommend rational antimalarial drug prescription in conformity with WHO/INRUD core drug prescribing indicators.
Downloads
Article Details
The journal grants the right to make small numbers of printed copies for their personal non-commercial use under Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported License.
References
1. Breman JG, Alilio MS, Mills A. Conquering the intolerable burden of malaria: What’s new, what’s needed: A summary. Am J Trop Med Hyg
2004; 71(2 Suppl):1‑15.
2. World Health Organization. World Malaria Report 2010. Geneva: World Health Organization, 2010. Available from: http://www.who.int/malaria/world_malaria_report_2010/en/index.html. [Last accessed on 2016 Dec 30].
3. World Health Organization. Guidelines for Treatment of Malaria. Geneva: WHO, 2010. Available from: http://www.whqlibdoc.who.int/publications/2010/9789241547925_eng, pdf. [Last accessed on 2016 Nov 17].
4. Sachs J, Malaney P. The economic and social burden of malaria. Nature 2002;415:680‑5.
5. Ridley RG. Medical need, scientific opportunity and the drive for antimalarial drugs. Nature 2002;415:686‑93.
6. Chima RI, Goodman CA, Mills A. The economic impact of malaria in Africa: A critical review of the evidence. Health Policy 2003;63:17‑36.
7. Goodman CA, Coleman PG, Mills A. Economic Analysis of Malaria Control in sub‑Saharan Africa. Geneva: World Health Organization, Global Forum for Health Research, 2000.
8. Yeung S, Pongtavornpinyo W, Hastings IM, Mills AJ, White NJ. Antimalarial drug resistance, artemisinin‑based combination therapy, and the contribution of modeling to elucidating policy choices. Am J Trop Med Hyg 2004;71(2 Suppl):179‑86.
9. Federal Ministry of Health. Nigerian national antimalarial treatment policy. Abuja, Nigeria: Federal Ministry of Health, 2005; 11.
10. World Health Organization: Framework for Developing Implementation and Updating Antimalarial Treatment Policy in Africa: A Guide for
Country Malaria Control Programme. Available from: http://www.afrolib.afro.who.int/documents/2003/english/framedrugp.pdf.
[Last accessed on 2016 Sep 28].
11. Abuaku BK, Koram KA, Binka FN. Antimalarial prescribing practices: A challenge to malaria control in Ghana. Med Princ Pract 2005;14:332‑7.
12. Mannan AA, Malik EM, Ali KM. Antimalarial prescribing and dispensing practices in health centres of Khartoum state, 2003‑04. East Mediterr Health J 2009;15:122‑8.
13. Meremikwu M, Okomo U, Nwachukwu C, Oyo‑Ita A, Eke‑Njoku J, Okebe J, et al. Antimalarial drug prescribing practice in private and public health facilities in South‑east Nigeria: A descriptive study. Malar J 2007;6:55.
14. Ogwal‑Okeng JW, Obua C, Waako P, Aupont O, Ross‑Degnan D. A comparison of prescribing practices between public and private sector physicians in Uganda. East Afr Med J 2004 2(Suppl):S12‑6.
15. Chapman S, Durieux P, Walley T. Good prescribing practice. In: Mossialos E, Mrazek M, Walley T, editors. Regulating Pharmaceuticals in Europe: Striving for Efficiency, Equity, and Quality. Milton Keynes, United Kingdom: Open University Press, 2004.
16. World Health Organization. How to Investigate Drug Use in Health Facilities: Selected Drug Use Indicators. EDM Research Series No. 007.
Geneva: World Health Organization, 1993.
17. Araoye MO. Sample size determination. In: Margaret OA, editor. Research Methodology with Statistics for Health and Social Workers. Ilorin: Nathadex Publishers, 2004; 115‑21.
18. Eze UI, Olowu AO. Prescribing patterns and inappropriate use of medications in elderly outpatients in a tertiary hospital in Nigeria. Trop J Pharm Res 2011;10:19‑25.
19. Irute John E, Ojieabu Winifred A, Patani‑Okolosi OE, Iwor Chioma P. Prescribing trends of antimalarial drugs in a primary health care facility in delta state. World J Pharm Res 2016;5:1‑10.
20. Abdo‑Rabbo A. Prescribing rationality and availability of antimalarial drugs in Hajjah, Yemen. East Mediterr Health J 2003;9:607‑17.
21. Afriyie D, Tetteh R. A description of the pattern of rational drug use in Ghana police hospital. Int J Pharm Pharmacol 2014;3:143‑8.
22. Fattouh R, Abu Hamad B. Impact of using essential drug list: Analysis of drug use indicators in Gaza Strip. East Mediterr Health J 2010; 16: 886‑92.
23. Awad A, Al‑Saffar N. Evaluation of drug use practices at primary healthcare centers of Kuwait. Eur J Clin Pharmacol 2010;66:1247‑55.
24. El Mahalli AA. WHO/INRUD drug prescribing indicators at primary health care centres in Eastern province, Saudi Arabia. East Mediterr Health J 2012;18:1091‑6.
25. Igboeli NU, Ukwe CV, Ekwunife OI. Increasing use of artemisinin‑based
combination therapy for treatment of malaria infection in Nigerian
hospitals. Pharm Pract (Granada) 2010;8:243‑9.
26. Igbiks T, Joseph O. Drug prescription pattern in a Nigerian tertiary
hospital. Trop J Pharm Res 2012;11:146‑52.
27. Bhavesh KL, Hiray RS, Ghongane BB. Drug prescription pattern of
outpatients in a tertiary care teaching hospital in Maharashtra. Int J
Pharm Bio Sci 2012;3:225‑9.
28. Koley M, Saha S, Arya JS, Choubey G, Ghosh S, Purkait R, et al.
A study on drug utilization and prescription habits of physicians in
a government homeopathic hospital in West Bengal, India. J Integr
Med 2013;11:305‑13.
29. Alyamani NA, Hopf Y, Williams DJ. Prescription quality in an acute
medical ward. Pharmacoepidemiol Drug Saf 2009;18:1158‑65.
30. Afriyie DK, Amponsah SK, Antwi R, Nyoagbe SY, Bugyei KA.
Prescribing trend of antimalarial drugs at the Ghana Police Hospital.
J Infect Dev Ctries 2015;9:409‑15.
31. Lenjisa LJ, Fereja HT. A retrospective analysis of prescribing practices
through WHO prescribing indicators at four selected hospitals of West
Ethiopia. J Bioanal Biomed 2014;6:29‑33.
32. Naseeb TA, Nasser MA. Drug prescribing indicators in primary health
care centers in Bahrain. Saudi Med J 2005;26:1436‑8.
33. Sunil K, Punam S, Madhuri K. Patterns of prescription and drug
dispensing. Indian J Pediatr 2005;72:117‑21.
34. Maïga MD, Diawara A. Study on the availability and cost of medicines
in the private sector in Mali. Med Trop (Mars) 2006;66:565‑8.