Recurrent Atelectasis in a Previously Healthy Child: A Case Report and Literature Review
Main Article Content
Abstract
Background: Atelectasis is the partial or complete collapse of a lung or its segment. The diagnosis of atelectasis in children calls for urgent identification and management of the underlying cause. There is a need for high index of suspicion of foreign body aspiration (FBA) in children with atelectasis even in the absence of a positive history. The aim of this report is to present a case of atelectasis from foreign body aspiration (FBA), without a suggestive history, in a previously healthy boy and review the relevant literature.
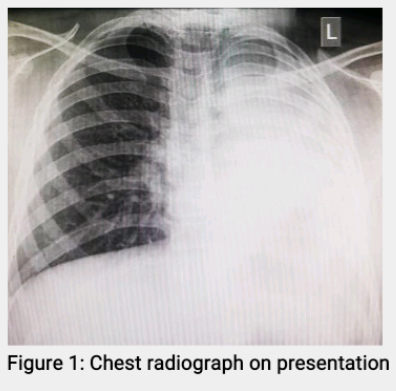
Case Report: A 10-year-old boy presented with a 2-week history of cough, weight loss and fever which failed to subside on out-patient treatment. He denied history of FBA. He was managed for left lobar pneumonia with lung collapse 3 months earlier with good response. He remained well till his re-presentation with features of recurrent left lobar pneumonia and lung collapse. He was re-admitted, re-evaluated, treated with remarkable improvement, then referred for further evaluation. Repeat chest CT identified foreign body (FB) in the airway and on rigid bronchoscopy, a biro end was extracted. Similar symptoms have not recurred.
Conclusion: Primary care providers and paediatricians must remain alert to FBA as a cause of atelectasis even in the absence of a positive history.
Downloads
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
The journal grants the right to make small numbers of printed copies for their personal non-commercial use under Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported License.
References
Grott K, Chauhan S, Sanghavi DK, Dunlap JD. Atelectasis. In: StatPearls. Treasure Island (FL): StatPearls Publishing, 2024.
Duggan M, Kavanagh BP. Atelectasis. In: Chernick V, Thomas F, Boat TF, Wilmott RW, Bush A, editors. Kendig's Disorders of the respiratory tract in children, seventh edition. Philadelphia, PA: W.B. Saunders, 2006; 616-621.
Peroni DG, Boner AL. Atelectasis: mechanisms, diagnosis and management. Paediatr Respir Rev 2000;1(3):274-278.
Sekerel BE, Nakipoglu F. Middle lobe syndrome in children with asthma: review of 56 cases. J Asthma 2004;41(4):411-417.
Tsai SL, Crain EF, Silver EJ, Goldman HS. What can we learn from chest radiographs in hypoxemic asthmatics? Pediatr Radiol 2002;32(7):498-504.
Hitter A, Hullo E, Durand C, Righini CA. Diagnostic value of various investigations in children with suspected foreign body aspiration: review. Eur Ann Otorhinolaryngol Head Neck Dis 2011;128(5):248-252.
Lutterbey G, Wattjes MP, Doerr D, Fischer NJ, Gieseke JJ, Schild HH. Atelectasis in children undergoing either propofol infusion or positive pressure ventilation anesthesia for magnetic resonance imaging. Pediatr Anesth 2007;17(2):121-125.
Luo Y, Wang Y, Gong K. Risk prediction model for long-term atelectasis in children with pneumonia. BMC Pulm Med 2023; 23(1):169.
Atağ E, Çakmak SC, Kalın S, Kaya B, Karakayalı B, Erdoğan S, et al. Etiology, diagnosis, and treatment in childhood atelectasis. Haydarpaşa Numune Med J 2021; 61(2):139-144.
Corrin B, Nicholson AG. Diseases of the conductive airways. In: Corrin B, Nicholson AG, editors. Pathology of the lungs, 3rd ed. Philadelphia, PA: Churchill Livingstone, 2011; 91-134.
Marchiori DM. Diseases of the airways. In: Marchiori DM, editor. Clinical imaging, 3rd ed. Maryland Heights, MO: Mosby, 2014; 1166-1177.
Romagnoli V, Priftis KN, de Benedictis FM. Middle lobe syndrome in children today. Paediatr Respir Rev 2014;15(2):188-193.
Eren S, Balci AE, Dikici B, Doblan M, Eren MN. Foreign body aspiration in children: experience of 1160 cases. Ann Trop Paediatr 2003;23(1):31-37.
Boufersaoui A, Smati L, Benhalla KN, Boukari R, Smail S, Anik K, et al. Foreign body aspiration in children: experience from 2624 patients. Int J Pediatr Otorhinolaryngol 2013;77(10):1683-1688. Mîndru DE, Păduraru G, Rusu CD, Țarcă E, Azoicăi AN, Roșu ST, et al. Foreign body aspiration in children-retrospective study and management novelties. Medicina (Kaunas) 2023;59(6):1113.
Foltran F, Ballali S, Rodriguez H, Sebastian van As AB, Passali D, Gulati A, Gregori D. Inhaled foreign bodies in children: a global perspective on their epidemiological, clinical, and preventive aspects. Pediatr Pulmonol 2013;48(4):344-351.
Na’ara S, Vainer I, Amit M, Gordin A. Foreign body aspiration in infants and older children: a comparative study. Ear Nose Throat J 2020;99(1):47-51.
Molla YD, Mekonnen DC, Beza AD, Alemu HT, Selamawi AE. Foreign body aspiration in children at University of Gondar Comprehensive Specialized Hospital, a two year retrospective study. Heliyon 2023;9(10):e21128.
Lowe E, Soylu E, Deekonda P, Gajaweera H, Ioannidis D, Walker W, et al. Principal diagnostic features of paediatric foreign body aspiration. Int J Pediatr Otorhinolaryngol 2024; 177:111846.
Destro F, Caruso AM, Mantegazza C, Maestri L, Meroni M, Pederiva F, et al. Foreign body ingestion in neurologically impaired children: a challenging diagnosis and management in pediatric surgery. Children (Basel) 2021; 8(11):956.
Liu B, Ding F, An Y, Li Y, Pan Z, Wang G, et al. Occult foreign body aspirations in pediatric patients: 20-years of experience. BMC Pulm Med 2020;20(1):320.
Cramer JD, Meraj T, Lavin JM, Boss EF. Object-related aspiration deaths in children and adolescents in the United States, 1968 to 2017. JAMA 2019;322(20):2020-2022.
Altuntaş B, Aydin Y, Eroğlu A. Complications of tracheobronchial foreign bodies. Turk J Med Sci 2016;46(3):795-800.
Hsu L, Green D, Chusid J, Talwar A, Shah R. Imaging of atelectasis. Contemp Diagn Radiol 2013;36(25):1-7.
Bhalla D, Naranje P, Jana M, Bhalla AS. Pediatric lung ultrasonography: current perspectives. Pediatr Radiol 2022; 52(10):2038–2050.
Ullmann N, D'Andrea ML, Gioachin A, Papia B, Testa MBC, Cherchi C, et al. Lung ultrasound: a useful additional tool in clinician's hands to identify pulmonary atelectasis in children with neuromuscular disease. Pediatr Pulmonol 2020;55(6):1490-1494.
Mahmoud N, Vashisht R, Sanghavi DK, Kalanjer S. Bronchoscopy. In: StatPearls. Treasure Island (FL): StatPearls Publishing, 2025.
Yavuz S, Sherif A, Saif S, Alzamar A, Alawad D, Abdelwahab A, et al. Indications, efficacy, and eomplications of pediatric bronchoscopy: a retrospective study at a tertiary center. Cureus 2023;15(6):e40888.
Safia A, Abd Elhadi U, Bader R, Khater A, Karam M, Bishara T, et al. Flexible versus rigid bronchoscopy for tracheobronchial foreign body removal in children: a comparative systematic review and meta-analysis. J Clin Med 2024; 13(18):5652.
Antón-Pacheco JL, Martín-Alelú R, López M, Morante R, Merino-Mateo L, Barrero S, et al. Foreign body aspiration in children: Treatment timing and related complications. Int J Pediatr Otorhinolaryngol 2021; 144:110690.