Pattern of cerebrospinal fluid analysis in children above the neonatal age as seen at the University of Port Harcourt Teaching Hospital
Main Article Content
Abstract
Background: Bacterial meningitis is a potent cause of morbidity and mortality in the paediatric age group.The aim of this study was to review the results of analysis the cerebrospinal fluid (CSF) collected from children above the neonatal age who were suspected to be having meningitis and to also determine the susceptibility pattern of these isolates.
Methods: A descriptive retrospective study of results of CSF culture reports taken from paediatric patients aged 1 month to 16 years with clinical suspicion of bacterial meningitis at the University of Port Harcourt Teaching Hospital between January 1, 2009, and December 31, 2014. The CSF samples were subjected to macroscopic examination, white blood cell count, Gram’s stain and culture. Organisms isolated were characterised by standard procedure and antibiotic susceptibility testing was done according to the Clinical Laboratories Standard Institute guidelines. Data were retrieved from laboratory record books and analysed using Microsoft Excel sheet. Results are presented as tables and pie chart.
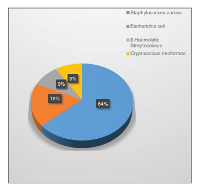
Results: Five hundred and seventy-four samples were received from children who were above the neonatal age (28 days). Of these, 329 were male (57.3%), 240 were female (41.8%), while in 5 (0.9%) of the samples, the sex was not indicated. Only 10 (1.7%) samples were positive for culture. Of these, Gram-positive cocci were the most common organisms, of which Staphylococcus aureus was the most prevalent, being 7 (70%), followed by Escherichia coli (20%), while the least prevalent organism was β-haemolytic streptococci (10%).
The organisms all exhibited resistance to amoxicillin-clavulanic acid. Ceftazidime exhibited 100% sensitivity against E. coli isolates. Ceftriaxone, cefotaxime and ciprofloxacin exhibited good sensitivity among all the bacteria isolates that were cultured.
Conclusions: There was a low yield of bacteria in CSF culture of paediatric patients at the University of Port Harcourt. The third-generation cephalosporins are still effective in bacterial meningitis in paediatric patients.
Downloads
Article Details
The journal grants the right to make small numbers of printed copies for their personal non-commercial use under Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported License.
References
1. Pérez AE, Dickinson FO, Rodríguez M. Community acquired bacterial meningitis in Cuba: A follow up of a decade. BMC Infect Dis 2010;10:130.
2. Prober CG, Srinivas NS, Mathew R. Central nervous system infections. In: Kliegman RM, Behrman RE, Jenson B, Stanton BF, editors. Nelson Textbook of Pediatrics. 18th ed. Philadelphia, PA: Saunders, 2007; 2936‑48.
3. Edmond K, Clark A, Korczak VS, Sanderson C, Griffiths UK, Rudan I. Global and regional risk of disabling sequelae from bacterial meningitis: A
systematic review and meta‑analysis. Lancet Infect Dis 2010;10:317‑28.
4. Theodoridou MN, Vasilopoulou VA, Atsali EE, Pangalis AM, Mostrou GJ, Syriopoulou VP, et al. Meningitis registry of hospitalized cases in children: Epidemiological patterns of acute bacterial meningitis throughout a 32‑year period. BMC Infect Dis 2007;7:101.
5. Dash N, Panigrahi D, Al Khusaiby S, Al Awaidy S, Bawikar S. Acute bacterial meningitis among children <5 years of age in Oman: A retrospective study during 2000‑2005. J Infect Dev Ctries 2008;2:112‑5.
6. Tikhomirov E, Santamaria M, Esteves K. Meningococcal disease: Public health burden and control. World Health Stat Q 1997;50:170‑7.
7. Ramakrishnan M, Ulland AJ, Steinhardt LC, Moïsi JC, Were F, Levine OS. Sequelae due to bacterial meningitis among African children: A systematic literature review. BMC Med 2009;7:47.
8. Kneen R, Solomon T, Appleton R. The role of lumbar puncture in children with suspected central nervous system infection. BMC Pediatr 2002;2:8.
9. Babalola AA, Coker AO. Pyogenic meningitis among Lagos children: Causative organisms, age, sex and seasonal incidence. Cent Afr J Med
1982;28:14‑8.
10. Johnson AW, Adedoyin OT, Abdul‑Karim AA, Olanrewaju AW. Childhood pyogenic meningitis: Clinical and investigative indicators of etiology and outcome. J Natl Med Assoc 2007;99:937‑47.
11. Baron EJ. Specimen collection, transport and processing. In: Jorgensen JH, Pfaller MA, Carroll KC, Funke G, Landry ML, Richter SS, et al.,
editors. Manual of Clinical Microbiology. 11th ed. Washington, DC: ASM Press, 2015; 76‑89.
12. World Health Organization. Laboratory Methods for the Diagnosis of Meningitis Caused by Neisseria meningitidis, Streptococcus pneumonia
and Haemophilus influenzae: WHO Manual. 2nd ed. Geneva, Switzerland: WHO, 2011; 432‑67.
13. Clinical and Laboratory Standards Institute (CLSI). Performance Standards for Antimicrobial Disk Susceptibility Tests; Approved Standards. CLSI DocumentM02‑A10. 10th ed. Wayne, PA: CLSI, 2009.
14. Nagarathna S, Veenakumari HB, Chandramuki A. Laboratory diagnosis of meningitis. In: Wireko‑Brobby G, editor. Meningitis. 2nd ed. China: InTech, 2012; 186‑208. Available from: http://www.intechopen.com/download/pdf/34329. [Last accessed on 2015 Oct 15].
15. OwusuM, Nguah SB, Boaitey YA, Badu‑Boateng E, AbubakrAR, Lartey RA, et al. Aetiological agents of cerebrospinal meningitis: A retrospective study from a teaching hospital in Ghana. Ann Clin Microbiol Antimicrob 2012;11:28.
16. Ogunlesi TA, Okeniyi JA, OyelamiOA. Pyogenic meningitis in Ilesa, Nigeria. Indian Pediatr 2005;42:1019‑23.
17. Sudharshan RC, Pradeep RM, Neelima R. Pattern and antibiogram of bacterial meningitis in children at a tertiary care hospital. J Sci Innov Res
2013;2:1012‑6.
18. Modi GB, Patel KD, Soni ST, Patel KJ, Mangukiya JD, Jain PS. Bacteriological profile of pyogenic meningitis in tertiary care hospital,
Ahmedabad. Natl J Med Res 2012;2:313‑7.
19. Yunusa T, Egah D, Banwat E, Shwe D, Kolade‑Yunusa O. Prevalence of H. influenzae among under‑five children presenting at the Emergency
Paediatric Unit (EPU) of two teaching hospitals in Jos, Plateau State,Nigeria. IOSR J Dent Med Sci 2014;13:73‑9.
20. Ibeawuchi R, Mbata T. Rational and irrational use of antibiotics. Afr Health Sci 2002;24:16‑8.